Meralgia Paresthetica is a condition that causes a burning, tingling, or abnormal sensation and pain in the thigh. Despite being a relatively common condition, I believe Meralgia Paresthetica is underdiagnosed and often confused with femoral nerve pain. In reality, what’s diagnosed as femoral nerve pain is actually pain or abnormal sensation coming from the Lateral Femoral Cutaneous Nerve instead.
If you have questions about this condition you’re in the right place. This blog is part 1 or 3 where I answer ALL your questions about Meralgia Paresthetica and the Lateral Femoral Cutaneous Nerve. In this one I’ll answer:
- What is Meralgia Paresthetica?
- What does the Lateral Femoral Cutaneous Nerve do?
- What does Meralgia Paresthetica feel like?
- Is Meralgia Paresthetica more common in certain people?
- What causes Meralgia Paresthetica?
- Can posture changes cause Meralgia Paresthetica?
If you’re struggling with Meralgia Paresthetica, make sure you read my other content. In it I discuss common symptoms, how it’s diagnosed, treatment options, and everything else you’re wondering about. Click on the links below and check out Part 2 and Part 3 for more information, including how to relieve it.
Part 2: Lateral Femoral Cutaneous Nerve Symptoms
- What are Lateral Femoral Cutaneous Nerve Symptoms?
- What are simple tests for Meralgia Paresthetica?
- Is burning in your thigh Meralgia Paresthetica or something else?
- Do I need an MRI if I have Meralgia Paresthetica?
- What conditions can mimic Lateral Femoral Cutaneous Nerve pain?
Part 3: Treatments for Meralgia Paresthetica
- What’s the best treatment for Meralgia Paresthetica?
- How can I relieve Meralgia Paresthetica at home?
- What are home treatments for Meralgia Paresthetica?
- What are medical treatments for Meralgia Paresthetica?
What is Meralgia Paresthetica?
Meralgia Paresthetica is a condition that causes a burning, tingling, or abnormal sensation and pain in the thigh. The abnormal sensation, called paresthesia, is a hallmark symptom of meralgia paresthetica. Burning and tingling in the front of the thigh results from compression of the lateral femoral cutaneous nerve (LFCN).
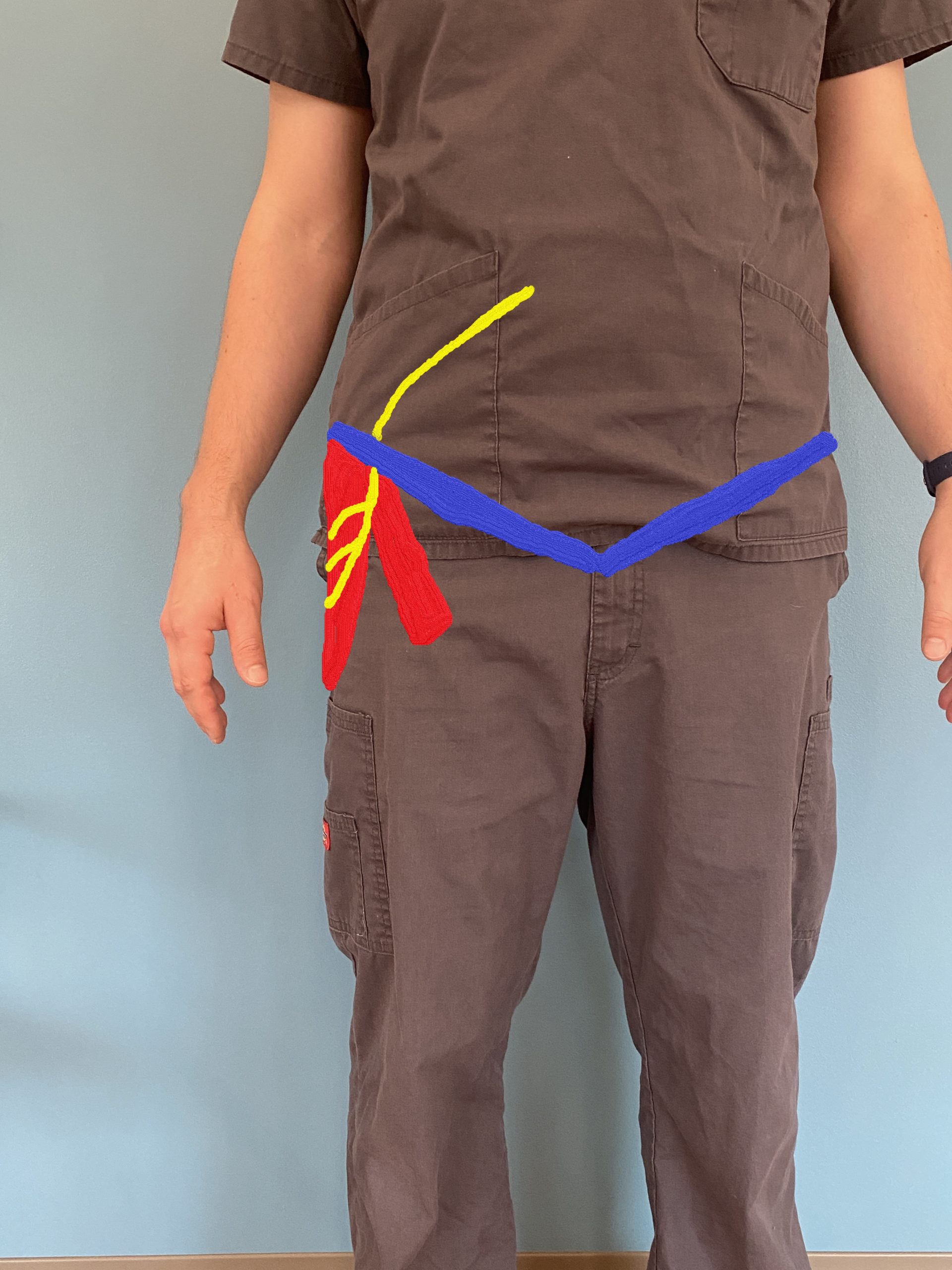
The lateral femoral cutaneous Nerve is a peripheral nerve with contribution from the L2 and L3 spinal nerve roots. After exiting the spine these lumbar nerves converge with others in a bundle, the lumbar plexus. The LFCN branches off and then runs through the pelvis, just laterally to the iliopsoas muscle.
Next, and importantly, the LFCN travels underneath the inguinal ligament. The inguinal ligament crosses over the front of the pelvis just above the front of the hip. After passing underneath the inguinal ligament it travels between the sartorius and tensor fascia lata (TFL) muscles. It continues and runs down the front of your thigh.
What Does the Lateral Femoral Cutaneous Nerve Do?
The LFCN provides sensation to the front of your thigh. You have one lateral femoral cutaneous nerve on each thigh. It’s purely a sensory nerve which means that it’s not involved in moving the thigh or leg. With meralgia paresthetica, the LFCN is most often compressed, underneath your inguinal ligament. It can also be compressed when it passes through your sartorius and TFL muscles.
What does Meralgia Paresthetica Feel Like?
Meralgia paresthetica usually feels like burning or tingling in the front of your thigh. Symptoms are usually only on one side, but you can have them on both sides. Although most lateral femoral cutaneous nerve pain feels like a burning or tingling, sometimes it’s also described as:
- Dull
- Aching
- Itching
- Buzzing
You may feel like the symptoms come and go, especially when you first start to notice them. If it persists, it sometimes becomes constant and is especially bothersome at night when trying to sleep. This can make sleeping frustrated and uncomfortable.
Is Meralgia Paresthetica More Common in Certain People?
If you’re having burning or tingling in the front of your thigh, you may be wondering if it’s the lateral femoral cutaneous nerve. First, it helps to know who most commonly experiences meralgia paresthetica. Here are a few key statistics about who experiences burning and tingling in the front of the thigh caused by meralgia paresthetica:
- It’s more common in middle-aged adults.
- Those with diabetes are six times more likely to have meralgia paresthetica.
- Men are three times more likely to have meralgia paresthetica than women.
It’s not necessarily meralgia paresthetica that’s causing thigh burning and tingling just because you fall into any of these categories. Looking at occupational factors that may cause compression of the lateral femoral cutaneous nerve is also helpful.
What Causes Meralgia Paresthetica?
As previously mentioned, meralgia paresthetica is caused by compression or stretch of your lateral femoral cutaneous nerve. What’s causing this compression or stretch on the nerve? Well, it can be quite a few things. Let me point out a few of the most common things that cause this condition:
- Wearing tool belts, duty belts, or body armor. These can compress your LFCN as it passes under the inguinal ligament.
- Tight clothing, especially tight pants or a belt that’s cinched tight will compress the area over the LFCN.
- Pregnancy, because of the weight and size of the expanding abdomen can cause meralgia paresthetica. Many women never had burning or tingling in their thighs before pregnancy.
- You may be prone to meralgia paresthetica after a c-section.
- If you have a BMI over 30 and carry more weight in your “belly” you may experience symptoms from the weight compressing the LFCN. This is especially true for those who might have gained weight quickly and noticed symptoms in their thighs that they didn’t have before the weight gain.
- Body-shaping compression sleeves that contour the abdomen may be causing compression of the LFCN.
- If you’ve been in a motor vehicle accident where you had your seatbelt on, the seatbelt can cause a compression injury to the area.
- Those who sleep on their stomach or are lying face down for an extended period of time (like during surgery) may have compression in the anterior thigh and hip over the LFCN.
- Athletes may be more predisposed because the sport they play leads to compression of the area or traction of the LFCN. Soccer, bodybuilding, gymnastics, and baseball athletes may be more likely to have Meralgia Paresthetica symptoms.
Can’t Sleep with Meralgia Paresthetica?
Read my recommendations on how to sleep with Meralgia Paresthetica. I cover the 3 best sleeping positions to relieve pain in the Lateral Femoral Cutaneous Nerve.
Can Posture Changes Cause Meralgia Paresthetica?
Besides lifestyle factors, you can also develop Meralgia Paresthetica from the traction of the LFCN based on mechanical factors like:
- Excessive anterior tilting of the pelvis. This is when your hips and butt move backward and you have an increased angle at your hip crease.
- A significant difference in the lengths between your two legs (more than just a few millimeters.)
As an aside, I’ve had a number of people ask me if Meralgia Paresthetica can be caused by a viral infection. I have not seen any evidence of this and I have not seen any evidence of this in the literature.

Jason Williams DC is a licensed Doctor of Chiropractic with Physical Therapy Modality and Acupuncture privileges. He is a chiropractor in Dumfries, VA at Sentara Therapy Center. Dr. Williams’ clinical expertise is in the evaluation, treatment, and rehabilitation of neuro-musculoskeletal conditions. Specific focuses include spinal, extremity, and sports-related complaints. He brings a patient-first attitude to his treatments and is a proponent of evidence-based and integrative care. See more content and his contact info here.
The opinions and views are mine personally, and do not necessarily reflect the views of others in the profession, my employer, or organizations that I belong to.